


Telemedicine, the practice of medicine through two-way voice or visual communication, is starting to become accepted as mainstream in Nevada. Since telemedicine began its current surge in popularity, technological updates, areas of practice and consumer demand all have been on the rise.
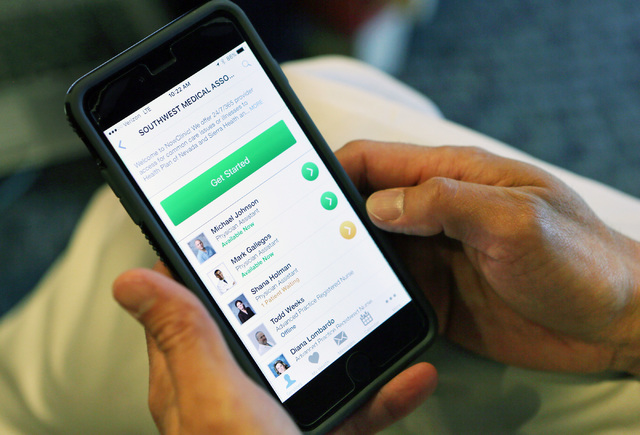
Dr. Eugene Somphone, medical director of on-demand care at Southwest Medical Associates, said the company is on track to see about 12,000 patients this year through video chat via smartphone or PC. That’s more than double the 5,000 patients who connected to Southwest Medical care providers remotely in 2014, the first year of operations it put the new tech to use on its electronic platform NowClinic.
Since then, NowClinic physicians have seen everything from simple rashes to colds, flus and bladder infections. The service is built around low-acuity cases involving some of the previously listed issues, along other nonemergency ailments. The number of patients seen through NowClinic is expected to continue to grow.
At inception, UnitedHealthcare’s Health Plan of Nevada and Sierra Health and Life plan’s 320,000 members were the only ones given access to NowClinic’s 24/7 service.
Since December, HPN’s SmartChoice Medicaid patients have had access to the system as well because the state made it legal for Medicaid patients to be seen electronically, Somphone said.
Starting in 2017, Somphone said, seniors registered under UnitedHealthcare’s Senior Dimensions, a Medicare Advantage plan, will be able to access NowClinic. This will increase the potential patient load for the electronic platform to 500,000, he said.
The use of telemedicine is a small but growing part of the health care services patients currently use, said John Jesser, president of LiveHealth Online at Anthem Inc.
Anthem, which owns and operates its Blue Cross and Blue Shield health plan in Nevada, rolled out its telemedicine platform, LiveHealth Online, not long after UnitedHealthcare’s move. Anthem provides its services through American Well, a Boston-based provider of online medical services. When Anthem launched its electronic platform, the insurer offered it to a wider audience than UnitedHealthcare had when it initially launched NowClinic in 2014. Along with giving access to many of its policyholders, Anthem also wants to offer access to family members, spouses and children of insured who are part of another health plan or are not covered at all, said Jesser. Jesser wouldn’t share exact numbers of usage rates but said the number of patients using its telehealth option has doubled since it launched in the first quarter of 2015.
Cost is another factor for telehealth. The cost of a visit through LiveHealth for people who aren’t direct plan members of Anthem is $49. Insured patients have a co-pay, which varies depending on their policy. This is a big savings for employees, said Jesser. The cost for patients using UnitedHealthcare’s plans is also low, with co-pays from zero to $20, said Somphone.
“Employers are very interested in this because they spend a lot of money on emergency-room visits,” said Jesser.
Visits to the emergency room can reach $1,000, and urgent-care costs hit around $200 “for some very simple things that could’ve been treated more directly through telehealth,” said Jesser.
Jesser also mentioned time savings for both employees who don’t have to leave work to see a doctor and employers who don’t have to be without the employee for several hours.
Convenience was also a part of why Anthem implemented telemedicine. There are times when a doctor is not readily available, such as the weekend, said Jesser.
Jesser said the other reasons were to create a better and affordable customer experience. Wait times are much lower. Somphone said the average wait time right now using NowClinic is about five minutes. A patient using the emergency room might wait three to five hours, he added.
Both Southwest Medical and Anthem are expanding the types of physicians available online. Both of the early adopters have launched an online psychology program. Anthem also recently enhanced its language capabilities with the launch of Cuidado Médico, which offers the choice to see a Spanish-speaking doctor using telemedicine.
The technology has gotten high ratings on both the physician side and the patient side since it was introduced, said Somphone. Critics add that there are dangers to using a remote system, but Somphone said providers are quick to send people on to higher-level care, such as the emergency room or quick care, if needed. For the most part, however, the patients who visit NowClinic are appropriate for the level of care telemedicine can offer — more than 95 percent, said Somphone.
Telehealth technology also is growing in capability. People with Anthem’s Medicaid plan, Amerigroup Nevada, now have access to a MedSuite kiosk at a Well Care Services facility near Boulder Highway and Tropicana Avenue.
There, patients see a doctor through an electronic platform inside a closed booth. But another layer is added to the care. The kiosk is equipped with biometric and peripheral devices: a digital thermometer, blood pressure monitor and dermatoscope, which adds to a physician’s diagnostic toolbox.
Some in the industry think there’s even more work to be done in advancing telemedicine technology. Dr. Samir Qamar, CEO and founder of MedLion, a direct primary care company, invented a device that increases the amount of care possible through telemedicine known as MedWand, which he now markets to hospitals and big insurers from his headquarters in Summerlin.
The device can plug into a PC, tablet or cellphone and contains an array of diagnostic tools. Some of the early tools put in the MedWand included a pulse oximeter, which measures the amount of oxygen in the blood; an otoscope camera for ear examinations; and attachments to view the eyes, throat and nose; an in-ear thermometer; a digital stethoscope; and a provision to support a third-party Bluetooth wireless device, such as a glucose meter or blood pressure monitor.
That list has been expanded to include several new options: a dermatoscope for the skin and nasoscope for the nose; a three-lead electrocardiogram; and a store and forward feature that keeps a memory, whereas the device only worked in real time before. The device also was given Bluetooth ingestion capabilities to bring data in from other devices, and a no-touch thermometer was added.
“My philosophy is that to make telemedicine successful as an industry, you have to replicate exactly what it would be in the clinical environment,” said Qamar.
Qamar said four areas of care need to be met to replicate what’s done at a physician’s office during an in person visit. The first is communication. This part has been done with the use of video interface companies. The second is examination. This is where the doctor might listen to the heart, lungs and other things of that nature. Third is testing. Qamar said he is designing something that will test blood from a remote area by way of a finger prick. And fourth is delivery of treatment to someone who is in a remote region.






